Birth Control - The Diaphragm
The IUD (intrauterine contraceptive device)
- What is “the IUD”?
- How does the copper IUD work?
- How effective is the copper IUD?
- Am I a good candidate for the copper IUD?
- Are there any reasons why I shouldn’t use the copper IUD?
- What are the common side effects of the copper IUD?
- What are the benefits of the copper IUD?
- When can the copper IUD be inserted?
- How is the copper IUD inserted?
- Are there any warning signs I should look out for after the IUD is inserted?
What is "the IUD"?
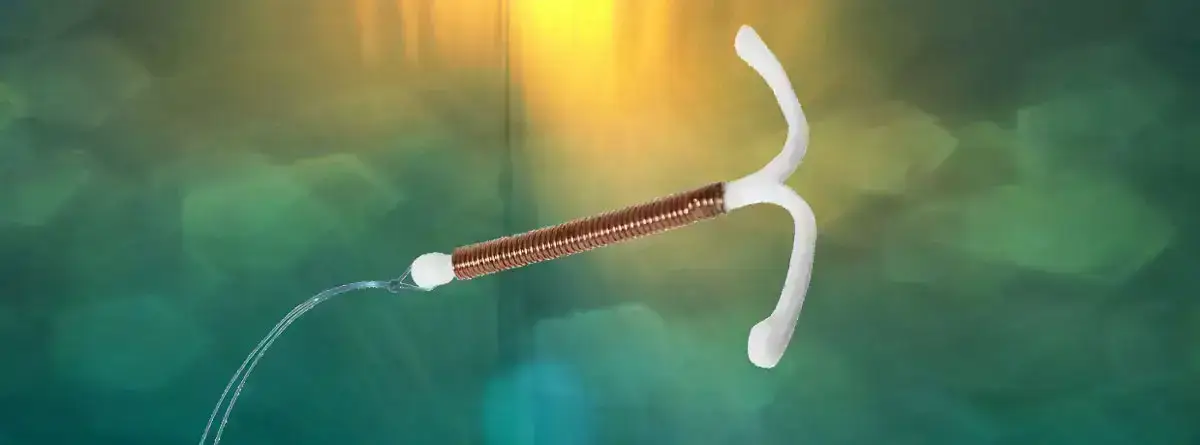
The IUD is a small, plastic device that is inserted by a physician / practitioner and left inside the uterus. Although there have been several types of IUDs, currently only two are available in the United States. Both are T-shaped and have a string at the base of the T that will extend trough the cervix and lie in the vaginal canal. The copper IUD releases a small amount of copper into the uterus and may remain in your body for up to 10 years. The hormonal IUD releases a small amount of the hormone progesterone into the uterus, but must be replaced every year.
How does the copper IUD work?
It primarily prevents pregnancy by interfering with the movement of sperm thus preventing fertilization of the egg. The copper IUD prevents fertilization as well as affecting the lining of the uterus so implantation will not occur.
How effective is the copper IUD?
The IUD is extremely effective. During the first year of use, 8 out of 1000 women will become pregnant with the Copper T.
Am I a good candidate for the copper IUD?
The copper IUD is best suited for women with families who want convenient, effective, reversible contraception. It is recommended for women who have at least one child, are in a stable, mutually faithful relationship (to minimize chance of exposure to sexually transmitted diseases that might cause pelvic inflammatory disease) and have no history or suspicion of pelvic infection.
Are there any reasons why I shouldn't use the copper IUD?
For some women, certain conditions can increase the chance of having problems with the IUD. The IUD may NOT be a good choice if you have:
- had a pelvic infection
- had an ectopic (tubal) pregnancy
- severe pain during menstrual periods
- abnormal vaginal bleeding
- multiple sexual partners or a high risk for sexually transmitted diseases
- allergy to copper
What are the common side effects of the copper IUD?
Irregular Bleeding:
- Bleeding problems constitute one of the more common IUD complications. Some women have cramping and spotting during the first few weeks after the IUD is placed. These should disappear within a month. The IUD does cause slightly crampier and longer menstrual periods. These symptoms can be treated with Motrin or Advil.
Pelvic Infection:
- The risk of developing a pelvic infection associated with the IUD is attributable to insertion of the device and exposure to sexually transmitted infection. The greatest risk occurs during the first few weeks following insertion. Women who have more than one sexual partner or whose partner has other sexual partners are at high risk for acquiring a sexually transmitted disease.
Expulsion:
- Between 2 and 10% of IUD users spontaneously expel their IUD within the first year. Expulsion, though infrequent, is more likely to occur during the first 3 months of use. An IUD expulsion can occur without a woman knowing it. Therefore, you should check regularly to make sure the “string” is still present.
What are the benefits of the copper IUD?
- highly effective
- easy to use — you don’t have to remember to insert it before sex or take a pill every day
- reversible — it can be easily removed in the office if you decide to get pregnant and you do not need to wait before attempting pregnancy can be used by breastfeeding women because there is no affect on lactation
- inexpensive — after the first year of use, the annual cost for using the IUD is less expensive per year may be used by women who cannot use hormonal methods and causes no systemic side effects (except in women allergic to copper or have a condition called Wilson’s disease)
- comfort – you should not be aware of the presence of the IUD. You and your partner should not be able to feel the IUD during intercourse
When can the copper IUD be inserted?
First it must be determined that you are a good candidate for the IUD. Your doctor will take a medical history, perform a pelvic exam and obtain any appropriate lab tests. The insertion can then be scheduled within the first 5 days of your next menstrual period; this insures that you are not pregnant at the time of insertion and the method is effective immediately for birth control. The IUD can also be placed after giving birth, as soon as your uterus has returned to its normal pre-pregnancy state. It can be determined whether you are ready for IUD insertion at your postpartum check.
How is the copper IUD inserted?
You may be given some antibiotics to take prior to insertion to protect from infection. Also, taking 3-4 Motrin or Advil an hour prior to insertion will minimize the discomfort of the insertion. Insertion of the IUD does not require anesthesia. Immediately before the IUD is inserted, you will be asked to sign a consent form making sure you understand everything about the insertion and a pregnancy test will be checked. To insert the IUD, the arms of the T-shaped device are folded and the IUD is placed in a long, slender, plastic tube. The tube is then inserted into the vagina and guided through the cervix into the uterus. The IUD is then pushed out of the plastic tube into the uterus and the tube is withdrawn.
Each IUD comes with a string or “tail” made of a thin plastic thread. After insertion the thread is trimmed so that 1-2 inches hang out of the cervix inside your vagina. You will be able to tell about the placement of the IUD by the location of the string. The string will not bother you, but your partner may feel it with his penis. If he reports discomfort, the string may be further trimmed. It is important that you check the string each month. To do this, you must insert a finger into your vagina and feel around for the string. You can do this at any time, but doing it after your menstrual period is easy to remember. If you feel the string is shorter or longer than it used to be-or if you don’t feel the string at all-call your doctor. The IUD may have slipped out of place. Use another form of birth control until your IUD is checked
Are there any warning signs I should look out for after the IUD is inserted?
Call your doctor if you have any of the following problems:
- severe abdominal pain
- pain during intercourse
- bleeding or spotting that occurs between periods, after intercourse, or that lasts more than a few months
- missed period or other signs of pregnancy
- unusual vaginal discharge
- a change in length or position of the string